Theme Lead: Professor Paul Murray
UL has strengths in the study of several oncogenic viruses, particularly Epstein-Barr virus (EBV) and human papillomavirus (HPV). Our overarching objective is to understand mechanisms underlying virus-driven transformation and to use this new knowledge to develop better treatments for the increasing global burden of virus-associated cancers, many of which are refractory to conventional therapies. The theme aligns with the overall LCRC strategy to understand the biology of cancer, and to identify new tools for early diagnosis and develop new treatments.
A) Contribution of virus genes and dysregulated viral life cycles to oncogenesis
A major goal is to understand the complex interplay between virus and host, particularly how ‘normal’ virus life cycles are perturbed during transformation and how these can be targeted therapeutically.
Murray’s group is investigating the contribution of dysregulated viral gene expression to B cell lymphomagenesis. These studies have defined novel latency-associated oncogenic viral programmes (appendix ref 1) and highlighted specific virus gene functions as therapeutic targets, for example, the viral GPCR/immunevasin, BILF1.
B) Dissecting therapeutically tractable cellular pathways regulated by oncogenic viruses
Many oncogenic viruses target cellular signalling pathways mutated in non-viral cancer forms. We are dissecting the contribution of oncogenic viruses to these deregulated cellular pathways and using this new knowledge to develop novel therapies.
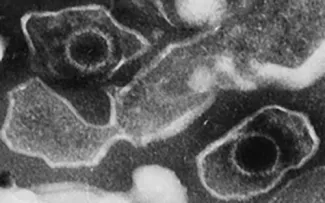
Murray’s group also focuses the role of viruses on the tumour microenvironment, including the interplay between EBV infection and inflammation. We have shown that collagen signalling is regulated by the EBV encoded oncogene, latent membrane protein-1 (FIGURE VO1) that contributes to tumour cell survival and chemo-resistance of B cell lymphomas (Cader et al., 2013). We have also shown that oncogenic lipid signalling through lysophosphatidic acid (LPA) regulates immune responses in EBV-associated cancers (Yap et al., 2015). Ongoing experiments are evaluating the efficacy of collagen and lipid signalling antagonists in syngeneic and humanised PDX models of B cell lymphoma.
We will develop new in vitro models to investigate chronic inflammatory tissue microenvironments and viral oncogenesis. Existing models based on end-stage disease do not provide information on early steps in pathogenesis. These new models will allow us to study how EBV and the microenvironment, including chronic inflammation, contribute to the early steps in EBV-associated carcinogenesis.
We will use these disease models to test novel antivirals. The viral genome and essential virus proteins are potential targets for drug-based therapies. Collectively, we will identify these targets and the optimal means to attack them. For example, EBV episome maintenance mediated by EBNA1 and suppression of the lytic cycle are as yet unexploited drug targets in EBV-driven cancers.
We will explore virus-host microbiome interactions and their contribution to oncogenesis. A better understanding of how the microbiome impacts on human cancer development requires a deeper appreciation of microbial interactions that constitute the ‘transkingdom’, a hitherto unexplored area. We will use our in vitro and animal models representative of the range of virus-associated malignancies to explore how oncogenic viruses interact with each other and with the host microbiome, and to determine how this promotes their transforming effects. Furthermore, although cross-sectional studies report associations between microbiota and cancer risk, response to therapy and patient outcome, we will use our large well-defined clinical cohorts with longitudinal samples and data, to ascertain which of these associations are clinically relevant.
We will exploit our expanding portfolio of NGS data to study the impact of virus sequence variation on disease outcomes. In collaboration with Professor Lawrence Young (University of Warwick) we are exploring using NGS data from our large patient cohorts, if virus sequence variation is associated with tumour development and/or clinical outcomes and to use our in vitro and in vivo models to dissect the impact of these sequence variations on transformation. In parallel, we will develop new tools to measure sequence variation that can be applied more routinely.
In the short term we will progress our studies with Dr Graham Taylor (University of Birmingham) to explore vaccination programmes for EBV-associated cancers and develop new combination trials. We will also expand our study of patients with other virus-associated malignancies, including patients with HPV-associated head and neck cancer (collaboration with Professor Ian Paterson, Universiti of Malaya)
In the medium term we will use our expanding portfolio of preclinical models to test the next generation of anti-viral drugs, including the repurposing of existing drugs as anti-virals.
In the longer term, we plan to explore the possibility of targeting novel 'lytic' transcripts, particularly, the EBV-encoded BILF1, a virally-encoded G Pprotein Coupled Receptor (GPCR).
Vockerodt M, Vrzalikova K, Ibrahim M, Nagy E, Margielewska S, Hollows R, Lupino L, Tooze R, Care M, Simmons W, Schrader A, Perry T, Abdullah M, Foster S, Reynolds G, Dowell A, Rudski Z, Krappmann D, Kube D, Woodman CBJ, Wei W, Taylor GM,. Murray PG. Regulation of S1PR2 by the EBV oncogene LMP1 in aggressive ABC-type diffuse large B cell lymphoma. J Pathol 2019; 248: 142-154.
Cader FZ, Vockerodt M, Bose S, Nagy E, Brundler M-A, Kearns P, Murray PG. The EBV oncogene LMP1 protects lymphoma cells from cell death through the collagen mediated activation of DDR1. Blood 2013 122; 4237-4245. SUBJECT OF BLOOD EDITORIAL- Carbone A, Gloghini A. Activated DDR1 increases RS cell survival. Blood 2013; 122: 4152-4.
Palser AL, Grayson NE, White RE, Corton C, Correia S, Ba Abdullah MM, Watson SJ, Cotten M, Arrand JR, Murray PG, Allday M, Rickinson AB, Young LS, Farrell PJ, Kellam P. Genome diversity of Epstein-Barr virus from multiple tumour types and normal infection. J Virol 2015; 89: 5222-37.
Lee HM, Lo KW, Wei W, Tsao SW, Chung GT, Ibrahim MH, Dawson CW, Murray PG, Paterson IC, Yap LF. Oncogenic S1P signaling in EBV-associated nasopharyngeal carcinoma activates AKT and promotes cell migration through S1P receptor 3. J Pathol 2017 242:, 62-72
Yap LF, Lai SL, Patmanathan SN, Gokulan R, Robinson CM, White JB, Chai SJ, Rajadurai P, Prepageran N, Liew YT, Lopes V, Wei W, Hollows RJ, Murray PG, Lambert DW, Hunter KD, Paterson IC. HOPX functions as a tumour suppressor in head and neck cancer. Sci Rep. 2016 Dec 9; 6: 38758. doi: 10.1038/srep38758
Li L, Li C, Mao H, Du Z, Chan WY, Murray P, Luo B, Chan AT, Mok TS, Chan FK, Ambinder RF, Tao Q. Epigenetic inactivation of the CpG demethylase TET1 as a DNA methylation feedback loop in human cancers. Sci Rep2016; 6:26591.
Patmanathan SN, Johnson SP, Lai SL, Panjabernam S, Lopes V, Wei W, Ibrahim MH, Torta F, Narayanaswamy P, Wenk MR, Herr DR, Murray PG, Yap LF, Paterson IC. Aberrant expression of the S1P regulating enzymes, SPHK1 and SGPL1, contributes to a migratory phenotype in OSCC mediated through S1PR2. Sci Rep 2016; 6:25650.
Saeed AA, Sims AH, Prime SS, Paterson I, Murray PG, Lopes VR. Gene expression profiling reveals biological pathways responsible for phenotypic heterogeneity between UK and Sri Lankan oral squamous cell carcinomas. Oral Oncol 2015; 51: 237-46.
Yap L-F, Velapasamy S, Lee H-M, Thavaraj S, Pathmanathan R, Wei W, Vrzalikova K, Khoo A, Tsao S-W, Paterson I, Taylor G, Dawson C, Murray PG. Downregulation of LPA receptor 5 contributes to aberrant LPA signalling in EBV-associated nasopharyngeal carcinoma. J Pathol 2015; 235: 456-65.
Murray PG, Young LS. An etiological role for the Epstein-Barr virus in the pathogenesis of classical Hodgkin lymphoma. Blood. 2019; 134:591-596
Vrzalikova K, Sunmonu T, Reynolds, G, Murray PG. Contribution of Epstein-Barr virus latent proteins to the pathogenesis of classical Hodgkin lymphoma. Pathogens 2018, 2018 Jun 27;7(3).
Vrzalikova K, Ibrahim M, Nagy E, Vockerodt M, Perry T, Wei W, Woodman C, Murray P. Co-Expression of the Epstein-Barr Virus-Encoded Latent Membrane Proteins and the pathogenesis of Classic Hodgkin Lymphoma. Cancers. 2018 Aug 24;10(9).