Researchers from University of Limerick and the UK have found that analysis of a newly described disease occurring in children linked to COVID-19 could allow doctors to better predict the outcome of young patients with this disease and develop new treatments for it.
Although children are less frequently affected by COVID-19 than adults, a new ‘hyperinflammatory syndrome’ in children associated with SARS-CoV-2 has emerged amongst some younger patients.
The new disease, known as Paediatric Inflammatory Multisystem Syndrome temporally associated with SARS-CoV-2 infection (PIMS-TS), shares many clinical features with a well-defined childhood illness known as Kawasaki disease, a leading cause of acquired heart disease in children caused by inflammation of the blood vessels.
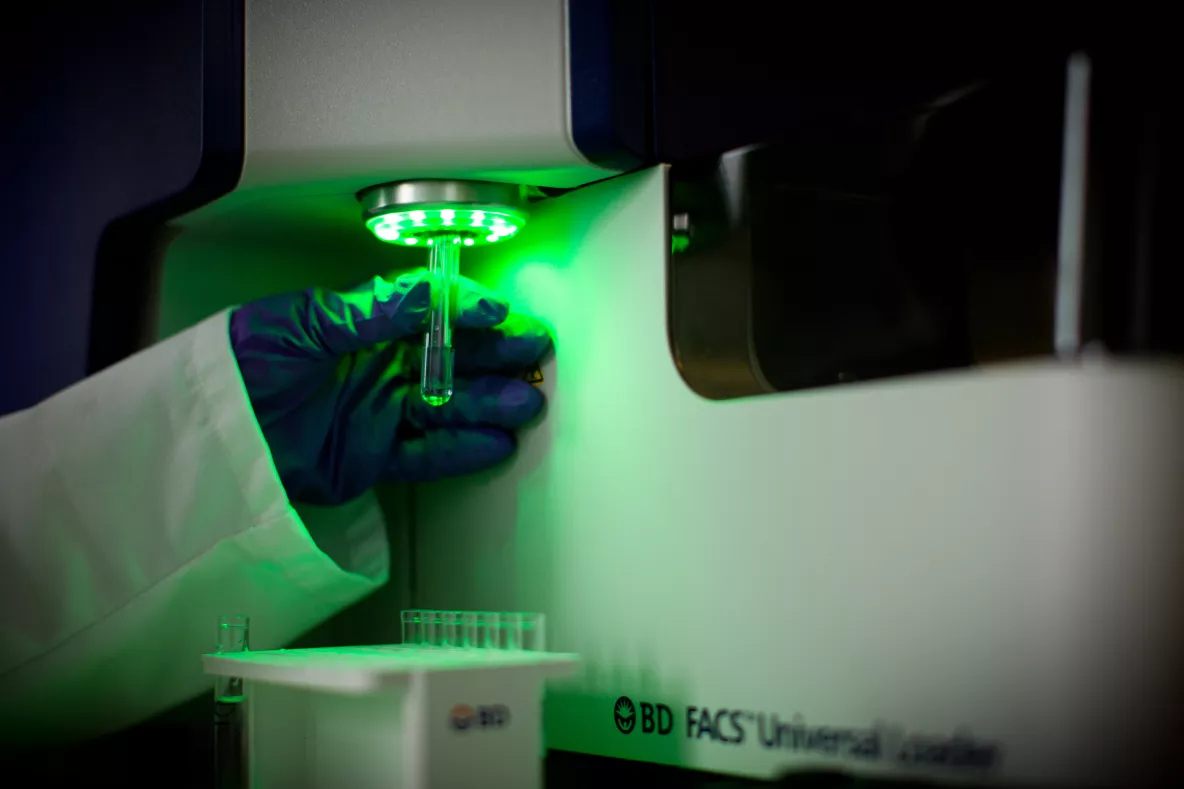
Experts in the study examined blood samples from children admitted with both diseases to Birmingham Women and Children’s Hospital during the UK’s coronavirus lockdown – discovering that large changes in the monocytes (a type of white blood cell) in patients with PIMS-TS and Kawasaki’s disease.
In this collaborative study, the researchers from University of Limerick, University of Birmingham and University of Warwick, together with health professionals from the NHS, used ground-breaking techniques to analyse single immune cells from the blood samples of children with PIMS-TS and Kawasaki disease.
The study found that a type of immune cell present in the blood, known as a monocyte (a white blood cell that is responsible for fighting infection), is vastly different in patients with PIMS-TS.
Dr Eanna Fennell, a post-doctoral fellow in the Health Research Institute at UL who pioneered the analysis of the single cell data, believes the study demonstrates the power of researchers from different fields coming together to tackle the COVID-19 pandemic.
“My training in computer based analysis of large and complex data allowed me to quickly identify the different forms of monocytes present in the patient’s samples and then to determine how different they are in PIMS-TS,” Dr Fennell said.
The study is the first to reveal that Kawasaki’s disease and PIMS-TS are both characterised by profound changes in the numbers of monocytes and their genetic make-up.
Paul Murray, Professor of Molecular Pathology in the Health Research Institute whose laboratory led the UL effort, highlighted the importance of this work in the context of the global fight against SARS-CoV2.
“This work represents a very significant advance in our understanding of this new coronavirus-associated disease and marks a vital step towards to the development of specific therapies for affected children.”
Vice President for Research at UL, Professor Norelee Kennedy said that “this exciting work by University of Limerick researchers, working with colleagues in the UK, demonstrates the value of an interdisciplinary approach to research and thus enhancing the understanding of how COVID-19 can affect some children".
Results of the study require confirmation in a larger patient cohort the group said, but the changes observed are likely to be highly relevant – potentially allowing doctors to predict the outcome for children with PIMS-TS and Kawasaki’s disease, as well as identifying alternative therapies for both diseases.
Researchers recruited nine children with signs of PIMS-TS presenting at Birmingham Women and Children’s Hospital to their study from April to May 2020. Seven met the UK’s Royal College of Paediatrics and Child Health case definition of PIMS-TS and were SARS-CoV-2 antibody positive. Two children fulfilled the criteria for diagnosis of Kawasaki’s disease and were SARS-CoV-2 antibody negative.
Ribonucleic acid (RNA) sequencing allowed experts to identify large changes in the frequency of classical, intermediate and non-classical monocytes occurring in both diseases.
SARS-CoV-2, the viral cause of COVID-19 usually causes mild respiratory infection in children and young adults. However, in rare cases, children subsequently develop PIMS-TS - presenting with fever, inflammation and evidence of organ failure resulting in cardiac dysfunction, hypotension and life-threatening shock.
Given the recent emergence of PIMS-TS, little is known about the immunological processes driving the disease and whether these are similar or different to Kawasaki’s disease.