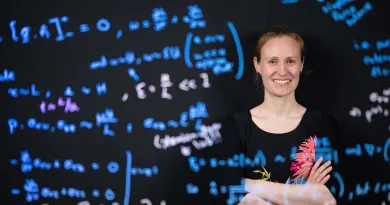
Aedín Culhane is Professor of Biomedical Sciences (Cancer Genomics) and Director of the Limerick Digital Cancer Research Centre in UL.
She is a computational oncologist with expertise in multi-omics data integration, statistical genomics, clinical bioinformatics and genomics in oncology. She has over 20 years experience in cancer genomics, of which over 15 years were in the Dana-Farber Cancer Institute and Harvard TH Chan School of Public Health in Boston, USA.
Her recent research focuses on algorithm development and integrative data of single cell molecular data in cancer to identify molecules that regulate and can be targeted during tumour development, progression, drug response and resistance. She is a leader in the Bioconductor community, a global open source, open development software in R for genomics and an advocate for open source science.

There’s so much to explore, so much to discover, but also, we can impact people. We can impact lives; we can save lives.
Professor Aedín Culhane is curious about cancer and how we can diagnose it, how we can prevent the disease, and how we can develop better treatments for cancer.
She’s trying to understand cancer at the single cell level, the real fine detail, trying to work out what exactly has gone wrong with the cancer cell, and also how we can use the cells or normal cells around the cancer cell to actually treat cancer.
Cancer and medicine are now a data science
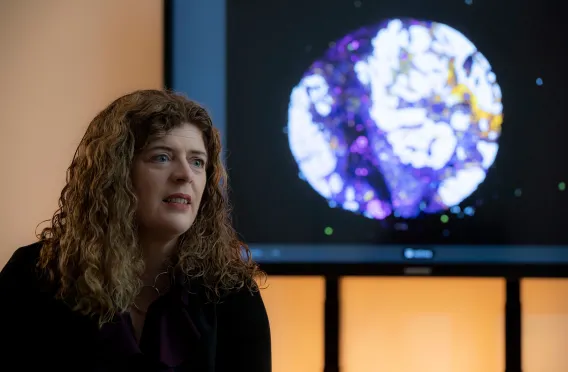
We are generating enormous amounts of data because the technology, like those microscopes to look at cancer, have got so much more detail down to the single cell level. And so that technology that's generating the labs then generates lots of data.
So, working in cancer harnesses expertise across disciplines from basic biology, bench biology in the lab, pathology, looking at the cells, of course the data science, the computer science, the AI, the machine learning that's required to analyse these vast amounts of learning and vast amounts of data.
And then bringing it the whole way back to the clinicians and the clinic because that's where we want the most impact.
The genome was sequenced about 20 years ago, but the actual final version of that genome wasn't actually available until last year. So, over the past 10, 15 years, we've been developing genomic tools, that's tools that can look at the genome. And these have been progressing and advancing and advancing and advancing. So, the tools we have today are far more detailed than what they were five or 10 years ago. And so, the data that we generate is obviously vastly more, so we can now generate information on every single cell, which is probably tens of thousands of cells in a single piece of tissue, and then on tens of thousands of genes. So, these are very, very large matrices of information and we need computers to analyse that information.
Delving into the unknown
The field that we work in, clinical cancer, computational biology is brand new. It didn't exist five or ten years ago. So, we're really developing a brand-new field because today we can take clinical samples and we can work with clinicians to identify cohorts of patient's forest study, and we can provide molecular data at such fine detail that we never could before, that we can really begin to interrogate the disease. That was impossible five years ago. That requires advanced mathematics, biostatistics, computational biology and machine learning in AI.
We're really bringing together many, many different fields to tackle this really important question. We work with people that come from a physics background. We work with biologists, we work with mathematicians with biostatisticians.
There are a number of people that come from various numerical fields to tackle this challenge. It creates a really vibrant research culture because we're experiencing so many different ideas together. And it really is that exciting field when you just get so many people that have so many different ideas together.

Data is paramount
One in two people in Ireland will be impacted by cancer. Around 43,000 people are diagnosed with cancer every year in Ireland, and one in three deaths in Ireland was from cancer. Every single family is impacted by this.
So, we are now at that point in time though, we can really begin to properly study and apply scientific methods to understand cancer. Prior to this, we didn't have the data, we didn't have the detail. Now we have it.
There's so much to explore, so much to discover, but also, we can impact people, we can impact lives, we can save lives. So, I spent fifteen years at Dana-Farber Cancer Institute in Boston, and I saw the changes over those 15 years when we started, when I started there most patients would be given a certain amount of time to live whereas now we see people that would have been given maybe three months to live 10 years ago, are now living happy, healthy lives with their families.
Research is always changing
I've seen that change in some cancers. We just may need to make that change for more cancers. For me, I think I always wanted to be exploring what was new. I always was excited by what was the next thing that was around the corner.
I did my UL co-op in San Francisco, in the Bay area in the 1990s when there was so much excitement about the emerging biotech industry. And that excitement then sort of gave me that realisation that we were on to something big.
For cancer, computational biology the big things have been the sequencing of the human genome and also the massive developments in computers in the internet, how we share data, how we analyse data. Without those two coming together, we wouldn't be doing this field. And if you think yourself of the changes that you've observed within the past five years in computers, going from paper maps to Google maps. Things that people relied on, 15-20 years ago are now defunct.
But cancer research has undergone that same change. So, the way that we do things now is completely different to how we did it ten or fifteen years ago because we have new tools because of the sequencing of the human genome and because of that we are using completely new ways to look at cancer and we need really bright, smart, motivated people to work with us because this is an enormous challenge.
Every single day there's another new paper that somebody has published in the field that changes how we think. So, you have to be ready to adapt. You have to be ready to talk to a lot of people because we don't work in silos. It's not like a group working in Limerick on their own. It's not even a group is working in Ireland on their own. We're immersed in a global community. So, it's important to like people and to like working with people and it's really important to be able to delve deep into a subject, understand it and advance the field.
Targeted approach for patient centred healthcare
In the 1980s and 1990s, most people got treated with chemotherapy and radiation. Chemotherapy and radiation target the fast-growing cells, like literally any fast-growing cells, cells that are dividing. That means that when you target cancer, we also lost our hair because our hair is growing. We targeted the immune system and there were a lot of side effects. There's a tonne of side effects from chemotherapy cause we're targeting not just the cancer cell but also the normal cells.
Now, can we actually design drugs that target the cancer specifically because then you won't have all of the side effects. And those side effects are so important to patients who are undergoing treatment because if the treatment makes you really sick, then you don't have the quality of life to spend with your family.
If we can give patients targeted therapy that's just targeting the cancer cells, then people can actually have a pretty normal good high quality of life with their families. And that's, that's what this is all about. It's all about impacting patients and their families.
In the past ten years there's been a lot of development of drugs that actually target specific mutations in the genes. And then more recently we're trying to use the body's own immune system to target cancer. So, as we learn more and more about the disease and also how it interacts with all the cells around it, we're developing more and more targeted therapies.
And as we develop more targeted therapies, we actually first of all do a better job of tacking the cancer cells. And secondly, patients have fewer side effects. Person-centred healthcare is our ability to take that disease and understand it in your context.
So, what is your disease? And then develop a medicine which will actually target your disease rather than using something like a broad chemotherapy and giving everybody the same treatment. So, the biggest impact that we can have for patients is if we increase the number of clinical trials that are available to patients. When patients are getting treated for cancer, they will have like the first line, the second line of therapy. And then at that point in time they're often looking for the new medicines, the thing that might actually treat their cancer.
The power of uniformity…
The eHealth hub for cancer is a funded programme from the HEA, [Higher Education Authority] in the shared island programme. This is an all-Ireland programme with UL Queens University Belfast leading.
One of the things that we're trying to do within the eHealth hub is connect health data, clinical health data on the island of Ireland. So, we can improve and increase the number of clinical trials available because we need to know how many patients are in Ireland that have a certain mutation and a certain type of cancer.
Because then we can design what we call an accrual plan. It's basically how many patients are likely to be in this trial. And that's really, really important. That data and that connected data is really important for clinical trials. And so that's what we're trying to do within the health hub for cancer.

We have connected into seven different cancer centres in Ireland. And what we are doing is working directly with clinicians, trying to see if we can harmonise the data. If we can get a harmonised local copy of their data and that data is in the same format as each hospital, we can now send a query to each one of those sites to then get statistics on the number of patients that are at each clinic, their genomics, what they're being treated for, and we can begin to get a better national picture of cancer in Ireland.
Collaborate for success
My greatest ambition is that we impact patients so that the research that we do improves the patient's experience of cancer in Ireland. We are working within a global community, like every single thing that we do is so much connected worldwide; with Northeastern and Dana Farber and John Hopkins in America, with researchers in Oxford and others across Ireland and Europe.
We add just small amounts to all of this global research, but together we can make a big impact. To me, healthy society is people living their best lives and particularly as people get older, that they are living their lives to their fullest, that they're enjoying their retirement with their families.
And for too many people, cancer impacts that it takes away years that they could otherwise enjoy communion and weddings that they could experience. So, if we can detect cancer early, we can treat it. If we can develop better medicines that work for patients in the clinic, then those people can go home and spend time with their families.
So, for me it's how our research in cancer computational biology can actually impact our understanding of cancer, and then patients.
World leaders
Within our team, we are leading community outreach for Bioconductor, which is one of the largest, global software projects for genomics. This field of understanding the genome and disease in health. For Bioconductor, we had over a million downloads last year from all over the world. We have about 2,000 active developers. We have a support site with 50,000 people registered from all over the world. And in UL we have the project which is leading that outreach globally. The Bioconductor community manager is training instructors all over the world in how to teach Bioconductor.
We really want to improve our outreach in Latin America, in Africa and in Asia where it's so important, particularly where they may not have traditionally had those computational biology skills. They now have the skills to analyse the genomics data that is coming from their own labs and is in turn is contributing to global projects.

They can now discover the nuances in the genome that are important for local diseases because the diseases that are important in western society are not the same diseases that are important in Sub-Saharan Africa where disease and infection is so important and where they need to understand the local genomes and the diversity of that genomes within Bioconductor.
We provide them the tools to actually analyse that genomic data. And when we asked our global community what they needed, they said training. And so that's what we're leading from our project here in UL is actually a global training for Bioconductor.
Open-source science is fundamental to the values in my lab and, and in what we do. We build on the knowledge of others, but also, we contribute to the global knowledge that's available and it's how we can all work together, not compete with each other, how we can work together to solve these bigger challenges like cancer. We are really just like a tiny pin in an enormous chain and everybody just adds to this effort.
From the local to the global
We need to move away from thinking of, this is Limerick versus Dublin versus Cork or any of this kind of local competitiveness. We really are tackling a much bigger challenge [in cancer] and we need to collaborate within Ireland, across the border. We need to collaborate within Europe, and we need to collaborate within the US.
We all need to work together to solve these problems. And that's what open source does. We all work with each other, we all share our code, we share our data and we build on the knowledge of others. The worst thing I think that puts so many people off science is they think it's only for like these incredibly smart people. Like, the Einsteins, the guy who jumps, "Eureka!" from the bath or something and that's not how science works at all.
It's much more methodical and it's much more iterative. It's building on what the previous person did. And we take it a little step forward and a little step forward and a little step forward!
And the importance is doing that each step. We're climbing a stairs, it's a really big stairs and we're taking it one step at a time. Nobody's leaping to the top. But actually, the person that sits there and just can actually do that work is actually just so important that we just need people who are engaged, who are motivated.

Playing to our strengths
I think UL has enormous strength in, in data analytics, in computer science. We've, got confirm here, we've got Lero [Research Ireland Centre for Software] here, we've got strengths in data science, we've got the data science CRT here, we've got a really strong Maths and Stats department. Researcher in the Bernal Institute and the Health Research Institute are collaborating, providing a really exciting environment to do research.
So those number skills are really critical in cancer computational biology. And those are the skills that brought me to UL because we need students who can actually think of these vast tables of numbers and data and actually make sense of them because each one of those rows is another gene in the cancer. And each one of those columns is a cell that's in a cancer. And we need to put all of that data together to understand what is driving cancer progression.
The Limerick Digital Cancer Research Centre (LDCRC) aims to use the newest, computer science, maths, statistics, our technology sensors to actually understand cancer.
It's how we can leverage strengths of UL, our strengths in development of nanomaterials, our strengths in biomaterials, our strengths in sensors, and then our strengths in data analysis, in computer science, in maths, and in stats to actually analyse the data in cancer and cancer data which has changed entirely in the past five to 10 years.
We now have the technology that actually can fine tune, understand cancers at the individual single cell level. And that generates vast amounts of data and vast amounts of data need maths, stats, computer science and AI to understand them. And by leveraging that strength of UL, we are advancing our understanding of cancer.
There's two major focuses of the LDCRC. One is in pathology - understanding the cancer on the slide, the tissue, and looking at that at the single cell level. Looking at every individual cell in the cancer and also all the normal cells surrounding it. The second is molecularly profiling, look at all the genes and proteins that are actually in that cancer. And that generates vast amounts of data for which we need the maths, the stats, and the AI.
So that second component is really the bioinformatics, the cancer computational biology, and it's how we can bring the best minds to actually analyse that data to develop cancer data science.
The LDCRC here in UL has a mission to understand cancer. It is using the strengths of UL in cancer research, strengths in data science and then also the tools that we use to interrogate cancer. So, we're using digital pathology, we're using sensors, we're using new technology so that we can understand the makeup of cancer and its detail at the molecular level.
Curious about Aedín Culhane's research

Read about the other researchers helping to change our society
Stay Curious for UL Research